Long-Term Effects of Clinical Ketamine Therapy On Brain Health
Schedule Your Ketamine Therapy Consultation Today
If you’re researching ketamine’s long-term effects on the brain, you may have found confusing or conflicting information. This is because much of the related content written about the effects of ketamine on the brain relate to the consequences of recreational abuse of the drug. These are fundamentally different scenarios from receiving carefully dosed IV ketamine treatments under medical supervision.
The effects of ketamine on the brain depend entirely on dose, frequency, route of administration, and context of use. In the medically therapeutic doses used to treat depression, research suggests ketamine supports brain health through enhancing neuroplasticity and resolving the executive functioning impairments that are core to depression. The brain changes associated with recreational abuse occur with doses that are 20-100 times higher than what’s used medically to treat depression, and taken far more frequently than treatments in a medical environment.
In this article, we examine what happens to the brain when exposed to ketamine over time under these two very different circumstances. It’s important to separate the science from the stigma.
Defining Ketamine Usages: Medical vs. Recreational
Before diving into brain effects, it’s essential to understand the distinction between IV ketamine used to treat depression in a safe, medical context and recreational ketamine abuse and misuse.
Medical Use of IV Ketamine for Depression
At Ember Health, we administer IV ketamine to treat Major Depressive Disorder (MDD) and the depressive state of Bipolar Disorder (BD). Ketamine is an FDA-approved anesthetic that has been used safely in medical settings for over 60 years. When used off-label for depression at sub-anesthetic doses, it offers rapid relief where traditional antidepressants have failed.
At Ember, the treatment involves carefully controlled intravenous infusions administered in a medical setting. Patients receive personalized dosing based on body weight, between 0.5 – 1.0 mg/kg, which usually results in approximately 50 mg for an average adult. That medication is delivered slowly over a 40-minute infusion. Care starts with a foundation of four infusions over 14 days. For the 84% Ember patients who experience relief of depressive symptoms following their foundation, care transitions to maintenance treatments approximately once every 6 weeks, as needed to maintain health and wellness goals.
At Ember, we conduct every infusion in a private suite with 1:1 medical monitoring by board-certified Emergency Medicine physicians or registered nurses. This focused attention on clinical safety and psychological support ensures patients experience the therapeutic benefits while minimizing any risks. At Ember Health, we’ve safely administered over 36,000 treatments using this approach.
Exposure to IV ketamine treatment in this way prompts the growth of new neural connections that help restore healthy mood regulation. Treatment goals are often to provide sustained relief from depression through the biological effects of ketamine and the neuroplastic changes it prompts in the brain. When integrated with ongoing psychotherapy and mental health care, IV ketamine can provide meaningful, lasting improvement and resolution of depressive symptoms.
Recreational Use of Ketamine
Recreational ketamine abuse represents a completely different scenario. In non-medical contexts, ketamine is often obtained from unclear or illegal sources and is sometimes mixed with other dangerous substances. Users typically consume ketamine through routes like snorted powder, oral lozenges, nasal sprays, or occasionally intramuscular injections – methods that make precise dosing impossible, significantly increase side effects, and increase risks of harmful outcomes.
Recent high-profile cases have brought recreational ketamine abuse into public awareness. In 2023, for example, Matthew Perry tragically died by drowning in a pool after consuming anesthetic levels of ketamine in an unsupervised environment. In 2025, British drag performer The Vivienne also died from polysubstance abuse with ketamine reportedly involved. Public figures like Elon Musk have discussed frequent, unmonitored ketamine use, raising real questions about recreational versus therapeutic contexts.
Recreational ketamine users often consume the drug daily in doses ranging from 1,000 mg to 12,000 mg per day (1-13 grams per day). This represents well over 20 times the dose used in a single medical treatment with Ember Health, where only patients receive the treatment once every 6 weeks on average. This means the cumulative exposure of ketamine misuse is often thousands of times higher compared to maintenance ketamine treatment in medical environments. When taken in unmonitored, often unsafe settings, these massive and frequent quantities of ketamine create serious risks for both immediate harm and long-term brain damage.
The FDA issued a warning in 2023 specifically about compounded ketamine products and the risks of unsupervised ketamine use. Recreational use often occurs in unpredictable environments from nightclubs to home settings, dramatically increasing the risk of accidents, and medical emergencies with no professional support available.
Head-to-Head Comparison of Medical vs. Recreational Ketamine
Understanding the differences between medical and recreational ketamine is essential for evaluating the impact of the drug on the brain:
Sources: Ember Health clinical protocols; FDA safety communications (2023); Marcantoni et al., Journal of Affective Disorders (2020)
Structural Changes: Ketamine Long-Term Effects on Brain Tissue Integrity
Ketamine’s effect on brain structure depends entirely on how it’s used. Medical ketamine promotes beneficial neuroplastic changes, while chronic recreational abuse causes neurotoxicity and can cause structural neural damage.
Therapeutic Use: Neuroplasticity and Brain Health
When used at medically appropriate doses and infrequent intervals, IV ketamine promotes beneficial changes in the brain. Research suggests these changes are the physical reversal of the prior harmful effects of chronic stress and depression, both of which negatively impact brain health.
Synaptic Growth and Connectivity
Research has demonstrated that therapeutic doses of ketamine rapidly increase synaptic density in the prefrontal cortex, the brain region involved in mood regulation, decision-making, and emotional processing. A landmark 2010 study in Science found that ketamine triggered the formation of new synaptic connections in mice, correlating directly with antidepressant effects.[1]
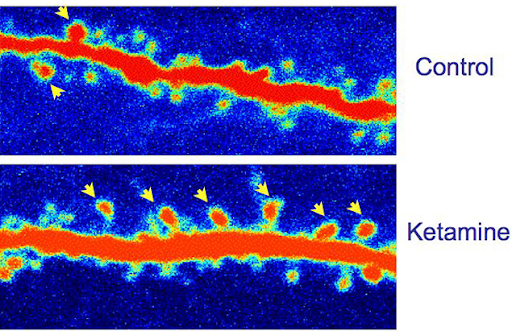
While translating animal studies to humans requires caution, neuroimaging studies in people receiving therapeutic ketamine have shown similar patterns of improvements. These changes appear to represent the reversal of prior synaptic loss caused by chronic stress and depression, essentially helping the brain rebuild healthy neural pathways.
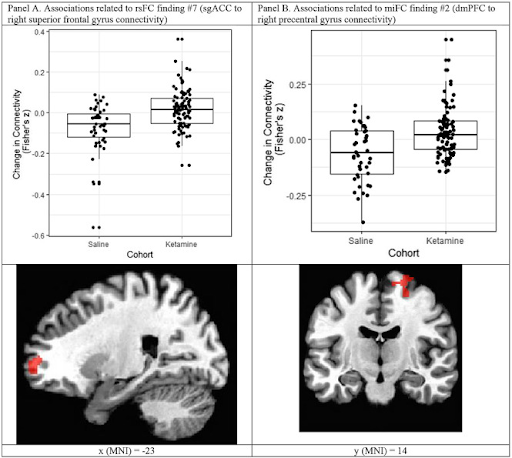
Rengasamy, Manivel et al.
eBioMedicine, Volume 99, 104902
Fig. 1 Examples of findings of changes in connectivity between ketamine and saline treatment groups. Dots represent values from individual participants and are jittered for ease of visualization. The lower and upper edges of the box correspond to the first and third quartiles (the 25th and 75th percentiles) and the horizontal line corresponds to the median. Each whisker extends from the edge of the box to the largest (for the top whisker) or smallest (for the bottom whisker) that is 1.5 times the interquartile range.
Imaging Studies Show No Structural Damage
Critically, controlled clinical studies of medical and therapeutic ketamine use have shown the potential for positive improvements in brain structure and cognition, with no adverse structural effects detected to date. MRI and other imaging studies of patients receiving appropriate medical doses show no gray matter loss, no white matter damage, and no signs of neurotoxicity.[5]
Short and medium-term studies (up to 2 years) consistently demonstrate that therapeutic ketamine, when administered under medical supervision with appropriate spacing between treatments, does not cause the structural brain changes associated with abusive consumption patterns.
In addition to the studies on physical brain structure, medical ketamine treatment has also shown improvement of cognitive function following ketamine exposure, highlighting the benefits of treating depression in this way.
Ketamine therapy offers evidence-based treatment for depression, anxiety, and other mental health conditions. Schedule a consultation call to learn more.
- Brooklyin Heights
- Chelsea
- Tribeca
- Upper East Side
- Williamsburg
Recreational Abuse and Misuse: Neurotoxicity and Structural Damage
In stark contrast, chronic ketamine abuse and misuse, characterized by daily use of high doses, has been associated with measurable negative structural brain changes.
Gray Matter Reductions
Multiple MRI studies have documented reduced gray matter volume in people who chronically abuse ketamine, particularly in frontal and temporal regions. A 2011 study in Biological Psychiatry found that individuals with chronic ketamine abuse (average use: 2.7 years at very high doses) showed significant gray matter reductions in areas involved in memory, attention, and emotional regulation.[6]
Importantly, these studies specifically examined people using 7,000-12,000 mg daily, doses 20 -100 times higher than the medical doses of ketamine for depression, with a cumulative ketamine exposure that is thousands of times higher than the doses in the treatment of depression. The structural damage correlates directly with cumulative exposure, and has not been observed in patients receiving medical ketamine at appropriate doses.
White Matter Integrity Changes
Diffusion tensor imaging (DTI) studies reveal that heavy recreational users show disruptions in white matter, the brain’s communication highways connecting different regions. Studies of individuals averaging 3 grams daily for 3+ years show measurable deterioration in white matter tracts, particularly those connecting frontal brain regions.[7]
Again, these changes only emerged after years of daily gram-level exposure, not from the carefully spaced 50 mg infusions used medically.
Important Context on Abuse Studies
Most studies of chronic recreational ketamine abuse have been conducted in Asian populations, particularly China, Hong Kong, and the UK, where recreational ketamine use is more prevalent. Additionally, recreational users often use multiple substances concurrently, which may confound findings. However, the consistency of findings across studies and the clear dose-response relationships support the validity of these observations.
The critical takeaway: these structural changes occur only at doses and frequencies that are orders of magnitude higher than medical use, and only in unmonitored, daily, chronic abuse scenarios.
Cognitive Outcomes: Ketamine Long-Term Effects on Brain Memory and Attention
The impact of ketamine on cognitive function, memory, attention, processing speed, and executive function, shows dramatically different patterns depending on dose and context.
The Therapeutic Angle: Cognitive Improvement
Research consistently suggests that cognition often improves as depression lifts with low-dose ketamine therapy. Dozens of studies support this finding.
When depression is severe, it impairs cognitive function across multiple domains. Patients struggle with concentration, memory, decision-making, and processing speed. As ketamine rapidly alleviates depressive symptoms, these cognitive improvements often follow.
Research examining cognitive outcomes in patients receiving therapeutic ketamine has found either improvement or stability across cognitive domains.[5] Studies specifically noted gains in:
- Attention and concentration – Patients report being able to focus more effectively on tasks
- Memory formation and recall – Both working memory and long-term memory often improve
- Processing speed – Mental tasks that felt laborious become easier
- Executive function – Planning, decision-making, and problem-solving improve
These improvements likely reflect both the direct relief from depression (which itself impairs cognition) and ketamine’s neuroplastic effects supporting healthy brain function. Importantly, studies following patients for up to 2 years show sustained cognitive benefits with appropriate maintenance treatment, with no evidence of cognitive decline from therapeutic ketamine use.
The Recreational Angle: Persistent Impairment Data
Chronic, high-dose recreational ketamine abuse tells a completely different story. Long-term cognitive risks are severe and can persist even after stopping use.
Specific, Enduring Cognitive Deficits:
Sources: Morgan et al., Addiction (2010); Longitudinal studies of chronic ketamine users[8]
Critical Context: These deficits correlate directly with cumulative lifetime ketamine exposure. Studies typically involve individuals who consumed thousands of grams over months or years, exposure levels thousands of times higher than a patient completing even years of maintenance ketamine therapy.
Longitudinal studies found that cognitive impairments persisted for at least one year after cessation in individuals with multi-year daily abuse.[8] Some evidence suggests partial recovery with sustained abstinence, but complete normalization is uncertain in severe chronic cases.
Beyond Cognitive Changes: Physical Risks
Chronic recreational ketamine abuse also significantly increases the risk of bladder damage. Ketamine cystitis (also called “K-bladder”) causes severe bladder inflammation, painful urination, and in extreme cases, bladder removal. This condition develops in chronic users consuming gram-level doses daily, and represents a serious medical consequence distinct from brain effects.
Psychiatric Risk & Benefit: Ketamine Long-Term Effects on Brain Emotional Stability
Ketamine’s impact on emotional regulation and psychiatric stability shows the same dose-dependent pattern seen with structural and cognitive outcomes.
The Therapeutic Angle: Sustained Mood Stability
Medical ketamine therapy provides sustained rapid antidepressant effects and supports long-term repair of the brain’s emotional reward system and balanced emotional regulation systems.
Rapid and Sustained Antidepressant Effects
Unlike traditional antidepressants that take weeks to months to work, ketamine often provides relief within hours to days. More importantly, with appropriate maintenance treatment, these benefits can be sustained long-term. Published meta-analyses show that approximately 75% patients in research trials experience relief from depression: 45% of patients achieve response (significant symptom reduction) and 30% achieve remission (minimal or no symptoms).[9]
At Ember Health, our clinical experience with over 36,000 treatments shows that a substantial majority of patients experience meaningful, sustained relief when ketamine is integrated into comprehensive care with ongoing psychotherapy and mental health support.
Repair of Emotional Regulation Systems
Depression doesn’t just cause sadness, it disrupts the brain’s entire emotional regulation system. The neural circuits involved in experiencing pleasure, processing rewards, managing stress, and maintaining emotional balance all become dysfunctional.
Therapeutic ketamine appears to help repair these systems. Patients describe:
- Experiencing pleasure and joy again in activities that once felt meaningless
- Improved ability to manage external stressors that previously felt overwhelming
- More balanced emotional responses rather than extreme swings
- Restoration of motivation and energy
- Reconnection with relationships and meaningful activities
These changes reflect ketamine’s neuroplastic effects supporting the rebuilding of healthy emotional circuitry, particularly when combined with psychotherapy during the “window” of enhanced neuroplasticity following treatment.
Long-Term Emotional Stability
With regular maintenance treatments and ongoing mental health care, patients often maintain these improvements long-term. The key is that ketamine provides a neuroplastic foundation that allows therapy, lifestyle changes, and other interventions to be more effective, creating sustained stability rather than temporary relief.
The Recreational Angle: Psychosis and Dependence
Chronic recreational ketamine abuse is associated with serious psychiatric risks that can undermine emotional stability and worsen underlying mental health conditions.
Psychosis-Like Symptoms
High-dose ketamine can produce dissociative and psychotic symptoms during acute intoxication. While these typically resolve as the drug wears off in one-time use, chronic abuse increases the risk of persistent psychosis-like symptoms including:
- Paranoid thinking and suspiciousness
- Hallucinations (seeing or hearing things that aren’t there)
- Delusions (fixed false beliefs)
- Disorganized thinking and speech
- Flat or inappropriate emotional responses
These symptoms may persist beyond acute intoxication in chronic abusers and can be difficult to distinguish from primary psychotic disorders.
Cognitive Distortions and Emotional Volatility
Beyond overt psychosis, chronic ketamine abuse is associated with problematic patterns of thinking and emotional instability:
- Distorted perceptions of reality
- Impaired judgment and insight
- Emotional numbness alternating with extreme reactivity
- Difficulty reading social cues and understanding others’ emotions
- Increased impulsivity and risky decision-making
Worsening of Underlying Mood Disorders
Perhaps most concerning, chronic ketamine abuse can worsen the very conditions that might have led someone to seek relief. Rather than treating depression, recreational abuse can:
- Deepen depressive episodes
- Trigger mania in predisposed individuals
- Increase suicidal thinking
- Worsen anxiety and panic
- Create a cycle where more ketamine is used to escape worsening mood, perpetuating the problem
This represents a clear irony: the substance that can treat depression when used medically can worsen depression and other mood disorders when abused.
Dependence Potential: Ketamine Long-Term Effects on Brain Tolerance and Addiction
The addiction and dependence potential of ketamine varies dramatically based on dose, frequency, and context of use.
The Therapeutic Angle: Low Dependence
Medical ketamine therapy, when administered at low doses in controlled clinical settings, shows minimal to no addiction potential.
Case Reports Only: Extremely Rare Occurrences
Dependence on therapeutic ketamine is so rare that virtually every instance becomes a published case report in medical literature. When something happens rarely enough that each occurrence warrants individual documentation and publication, it tells you the phenomenon is exceptionally uncommon.
The medical literature contains occasional case reports of patients developing problematic patterns with prescribed ketamine, but these cases typically involve:
- Doses higher than medically accepted standard protocols
- More frequent administration than recommended (usually daily)
- Lack of appropriate psychological screening or monitoring
- Poly substance use history
- Self-administration rather than clinically supervised use
At Ember Health, with over 36,000 treatments administered using strict protocols, appropriate doses, appropriate spacing (once every 6 weeks on average for maintenance), and mandatory mental health provider collaboration, we have not observed problematic dependence patterns.
Why Medical Ketamine Has Low Addiction Potential
Several factors explain the minimal addiction risk in therapeutic, medical settings:
- Low doses – 50 mg doses don’t produce the euphoria or dissociation that drives recreational use
- Infrequent administration – Treatments spaced weeks apart don’t allow tolerance or dependence to develop
- Medical supervision – 1:1 monitoring, and only administered in office by a medical professional
- Integrated care – Required mental health provider involvement addresses underlying issues
- No self-administration – Patients cannot increase doses or frequency on their own
- Limited source policy – At Ember Health, we require that patients in our care confirm they are not receiving ketamine from any other sources.
The addiction potential that exists with ketamine emerges only with much higher doses, frequent use, and self-administration, all factors explicitly absent in medical protocols.
The Recreational Angle: Addiction and Systemic Damage
Recreational ketamine abuse carries significant risk of rapid tolerance, rapid dependence, and severe side effects including ketamine cystitis (K-Bladder).
Rapid Tolerance Development
When ketamine is used recreationally at high doses, tolerance develops quickly. Users find that the same dose no longer produces the desired effects, leading them to increase doses progressively. This escalation is what causes people to consume grams per day, doses that would be equivalent to surgical anesthesia levels in a ketamine-naive individual before abuse began.
This tolerance-driven dose escalation creates a dangerous cycle:
- Initial recreational doses of 100-500 mg produce desired effects
- Within weeks to months, users need 1,000+ mg for the same effect
- Eventually, daily consumption reaches 3,000-12,000 mg
- At these levels, serious medical complications become likely
Rapid Dependence
Beyond tolerance, psychological and physical dependence develop quickly with regular recreational use. Users experience:
- Cravings – Intense desire to use ketamine
- Loss of control – Inability to limit use despite wanting to stop
- Continued use despite harm – Using even as health, relationships, and functioning deteriorate
- Withdrawal symptoms – Anxiety, depression, insomnia, and intense cravings when not using
The compulsive pattern of use, combined with tolerance requiring higher doses, creates the conditions for serious medical complications.
The Addiction Cycle
The progression typically follows this pattern:
- Recreational use begins (100-500 mg doses)
- Tolerance develops (doses increase to 1,000+ mg)
- Dependence emerges (daily use becomes compulsive)
- Physical complications begin (cognitive issues, K-Bladder symptoms)
- Doses escalate further to cope with worsening problems
- Severe medical and psychiatric consequences develop
Breaking this cycle requires professional addiction treatment, often including medical detoxification, psychiatric care, and long-term recovery support.
A Word from Ember Health: Our Focus on Patient Safety and Clinical Protocols
At Ember Health, we’re committed to precise therapeutic ketamine dosing protocols and comprehensive monitoring. Our treatment strategy is explicitly designed to maximize neuroplastic benefits while actively mitigating long-term risks associated with unsupervised use.
Our Safety Approach:
- Precise dosing: 0.5 -1.0 mg/kg IV (approximately 50 mg), personalized to body weight
- 1:1 medical monitoring: Board-certified Emergency Medicine physicians and RNs present throughout every treatment
- Appropriate frequency: 2x per week during induction, then on average every 6 weeks for maintenance, spacing that prevents tolerance
- Continuous monitoring: Clinicians present to monitor heart rate, blood pressure, oxygen, and respiratory rate as needed
- Private infusion suites: Calm, comfortable environments designed for safety and psychological support
Over 36,000 Treatments Done Safely: Our extensive experience demonstrates that appropriately dosed, medically supervised ketamine therapy is both safe and effective.
Long-Term Monitoring Core to Our Care: We track outcomes through bi-weekly digital mood surveys, regular clinical reassessment, and collaborative communication with each patient’s mental health provider. Treatment frequency is individualized based on response, and we continuously monitor for any changes in cognitive function or overall wellbeing.
Mandatory Mental Health Collaboration: All patients work with a licensed mental health provider. Ketamine is most effective when integrated into comprehensive care including psychotherapy, lifestyle modifications, and other evidence-based interventions.
Our protocols are informed by the largest global dataset on IV ketamine for depression and ongoing partnership with Harvard researchers, ensuring our approach reflects the latest evidence while prioritizing patient safety.
Final Takeaway: Navigating Ketamine Long-Term Effects on Brain Safety
Risk is Dose, Route, Frequency, and Context-Dependent
The evidence is clear: ketamine’s effects on the brain depend entirely on how it’s used.
Therapeutic use leads to sustained neuroplasticity:
- Low doses (0.5 – 1.0 mg/kg IV) administered infrequently (every 6 weeks on average)
- Intravenous route with medical supervision and 1:1 monitoring
- Integration with mental health care
- Result: Beneficial brain changes, synaptic growth, improved emotional regulation, cognitive enhancement, without structural damage or neurotoxicity over years of care
Chronic misuse causes neurotoxicity and structural damage:
- High doses (1,000-12,000 mg daily) used daily or multiple times a week
- Non-medical routes (snorted, oral) in unmonitored settings
- Often combined with other substances
- Result: Gray matter loss, white matter damage, persistent cognitive deficits, emotional instability, psychosis risk, rapid dependence, and K-Bladder
The difference is categorical. Research on recreational abuse cannot be translated to medical ketamine regimens. They are fundamentally different exposures with fundamentally different outcomes.
Seek Licensed, Experienced Clinicians
If you’re considering ketamine therapy for depression, the evidence strongly supports its safety and effectiveness when provided by licensed, experienced clinicians who adhere to strict safety and dosing protocols. The same substance that causes devastating brain damage when abused recreationally can support neuroplasticity and recovery when used medically. Make sure you receive care from experienced clinicians who understand this distinction and maintain the protocols necessary to ensure your safety.
Frequently Asked Questions
Will therapeutic ketamine cause brain damage?
No. Current clinical evidence shows that therapeutic, low-dose, supervised ketamine use does not causes brain damage. Neurotoxicity is associated with high-dose, chronic recreational abuse.
Are the positive neuroplastic changes from ketamine permanent?
The synaptic growth is rapid, but the long-term benefit for mood typically requires ongoing maintenance therapy and integration with psychotherapy. Ketamine helps regrow neurons, but the brain can lose to new neurons to new stress and trauma.
How long does the cognitive impairment from recreational ketamine last?
Cognitive deficits (especially memory and attention) from chronic, high-dose abuse can persist for years or may even be permanent in severe cases, even after abstinence.
Medical Disclaimer
This information is for educational purposes and does not replace medical advice. IV ketamine for depression is an off-label use of an FDA-approved medication. Ember Health requires medical screening and that patients to work with a licensed mental health provider as part of their comprehensive care plan. Treatment outcomes vary significantly by individual. All treatments are administered in medically supervised settings with 1:1 patient-to-clinician ratios.
References
[1] Li N, Lee B, Liu RJ, et al. mTOR-dependent synapse formation underlies the rapid antidepressant effects of NMDA antagonists. Science. 2010 Aug 20;329(5994):959-64. https://pubmed.ncbi.nlm.nih.gov/20724638/
[2] Abdallah CG, Averill LA, Gueorguieva R, et al. Modulation of the antidepressant effects of ketamine by the mTORC1 inhibitor rapamycin. Neuropsychopharmacology. 2020;45(6):990-997. https://pmc.ncbi.nlm.nih.gov/articles/PMC7162891/
[3] Chen MH, Li CT, Lin WC, et al. Rapid inflammation modulation and antidepressant efficacy of a low-dose ketamine infusion in treatment-resistant depression. Molecular Psychiatry. 2024;29(1):162-170. https://www.sciencedirect.com/science/article/abs/pii/S0165178118300623
[4] Kim JW, Monteggia LM. Increasing doses of ketamine curtail antidepressant responses and suppress associated synaptic signaling pathways. Behavioural Brain Research. 2020;380:112378. https://pubmed.ncbi.nlm.nih.gov/31760154/
[5] McIntyre RS, Rosenblat JD, Nemeroff CB, et al. Synthesizing the evidence for ketamine and esketamine in treatment-resistant depression: an international expert opinion. American Journal of Psychiatry. 2021;178(5):383-399. https://pubmed.ncbi.nlm.nih.gov/33726522/
[6] Liao Y, Tang J, Corlett PR, et al. Reduced dorsal prefrontal gray matter after chronic ketamine use. Biological Psychiatry. 2011 Jan 1;69(1):42-8. https://pubmed.ncbi.nlm.nih.gov/21035788/
[7] Liao Y, Tang J, Fornito A, et al. Alterations in regional homogeneity of resting-state brain activity in ketamine addicts. Neuroscience Letters. 2011;522(1):36-40. https://pubmed.ncbi.nlm.nih.gov/22698584/
[8] Morgan CJ, Muetzelfeldt L, Curran HV. Consequences of chronic ketamine self-administration upon neurocognitive function and psychological wellbeing. Addiction. 2010;105(1):121-133. https://pubmed.ncbi.nlm.nih.gov/19919593/
[9] Marcantoni WS, Akoumba BS, Wassef M, et al. A systematic review and meta-analysis of the efficacy of intravenous ketamine infusion for treatment resistant depression. Journal of Affective Disorders. 2020;277:831-841. https://pubmed.ncbi.nlm.nih.gov/33065824
[10] American Psychiatric Association. Consensus Statement on the Use of Ketamine in the Treatment of Mood Disorders. 2017. Available at: https://www.psychiatry.org/psychiatrists/practice/professional-interests/ketamine
[11] Veterans Affairs/Department of Defense Clinical Practice Guideline for the Management of Major Depressive Disorder. 2022. Available at: https://www.healthquality.va.gov/guidelines/MH/mdd/
[12] Alnefeesi Y, Chen-Li D, Krane E, et al. Real-world effectiveness of ketamine in treatment-resistant depression: A systematic review & meta-analysis. Journal of Psychiatric Research. 2022;151:693-709. https://pubmed.ncbi.nlm.nih.gov/35688035/
[13] U.S. Food and Drug Administration. FDA warns consumers not to use compounded drugs containing ketamine. Safety Communication. October 2023. Available at: https://www.fda.gov/drugs/drug-safety-and-availability/
[14] Dai, D., Miller, C., Valdivia, V. et al. Neurocognitive effects of repeated ketamine infusion treatments in patients with treatment resistant depression: a retrospective chart review. BMC Psychiatry 22, 140 (2022). https://doi.org/10.1186/s12888-022-03789-3




%20for%20Depression.avif)

